Abstract
In implant dentistry osseointegration is referred as the contact between bone andimplant, without interference of non-bone tissue in between. It has been documented thatpresence or absence of osseointegration will lead to the success or failure of the rehabilitation. There are several factors that will determine if the dental implant can integrate well within the bone of the patient. Metabolic diseases,habits of the patient, the quality and quantity of the bone and the micro and macrotopography of the implant that is used, are factors that will highly influence the osseointegration of the implant.
1. Introduction
The term osseointegration was first incorporated by Dr. Per-Ingvar Branemark, who is considered the father of modern dental implantology. Branemark defined osseointegration as "direct contact between the bone and metallic implants, without interposed soft tissues layers".
Dr. Branemark made this discovery while performing orthopedic experiments on rabbit legs where he inserted titanium implants. He uncovered the remarkable bio-compatibility of the material with the bone and this lead to the concept of osseointegration and their upcoming studies.
Zarb and Albrektsson defined osseointegration as "a time dependent healing process whereby clinically asymptomatic rigid fixation of alloplastic materials is achieved and maintained in bone during functional loading".
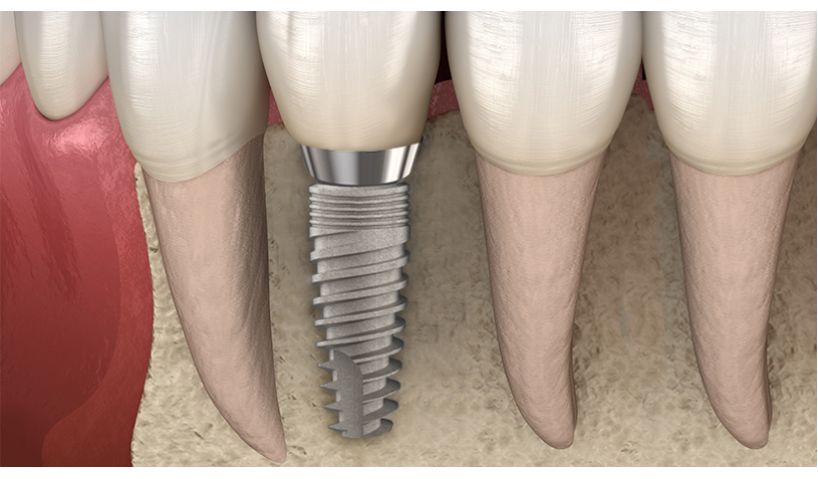
Therefore, osseointegration is simply a direct relation between the bone and the implant, where an interlocking between the implant and the bone exists.
According to Parithiarklaignan et. al osseointegration has 3 stages: the incorporation of the implant by woven bone formation, adaptation of the bone mass to the load and adaptation of the bone structure to load.
The primary stability and the fixation of an implant depends of the geometry, diameter, length, thread designand surface topography.
There have been several studies that shows that the length of the dental implant is not so relevant as was thought in the past. Ajayi et al. showed that short dental implants providesviable outcomes in teeth replacement.
The geometry of most implants is similar these days, so the focus has shifted to the surface treatment.Schwartz et al. has mentioned that the surface modification affects the adhesion of the cells to the implant, as well as the propagation and the protein adsorption at the initial stages of healing.
Buser et al. described that one of the key factors that affects the speed of the osseointegration is the characteristics of the surface of implants; rough surfaces promotes a faster osseointegration due to the mechanical fixation.
Ting Ma et. al has stated that SLA surface treatment is the "gold standard" for surface modifications of dental implants.
2. Factors that affect osseointegration of dental implants
Among the many factors that affect the osseointegration, the most important ones are probably the geometry and the surface of the implant.
Other potential factors are:
- Bone quantity – the amount of bone surrounding the implant. 7
- Bone quality - the type of bone and its density
- Loading conditions and healing time.
- Implant material.
- Smoking.
- Systemically compromised patients.
- Diabetes.
- Heat generated by lack of irrigation during the procedure or due to old dental burs (temperature can produce necrosis of the tissue).
- Skill of the surgeon.
3. Conclusion
There are many factors that enhance theosseointegration of a dental implant, a skilled surgeon using a dental brand with the correct geometry, surface treatment along with a good receptor site will achieve a predictable result. Osseointegration should be the main goalof the Doctor and of the companies providing dental implants,the characteristics of the implant will be criticin patients who lacksbone quality and quantity, considering that this situation is found in most of the patients.
Evidence has shown that the geometry of the implants is almost the same for most of the producing companies, also has been demonstrated that the length may not be as important as it was thought. Because of this reason, the clinician should focus on the surface treatment of the implant that is being used. It is well known that SLA surface modification is not only as good as other kinds of surface treatments in short term but is even better on the long-term data.Therefore, this type of implants should be chosen in combination of a good study of where and how the implant is going to be placed to provide the patient with the best possible outcome.
References
- Branemark R, Branemark PI, Rydevik B, Myers RR. Osseointegration in skeletal reconstruction and rehabilitation: A review. JRRD 2001;38(2):175-81.
- Kim, T.-I. A tribute to Dr. Per-Ingvar Brånemark. Journal of Periodontal & Implant Science, 2014. 44(6), 265. http://doi.org/10.5051/jpis.2014.44.6.265
- Zarb GA, Albrektsson T. Nature of implant attachments. In: Branemark P-I, Zarb C, Albrektsson T, editors. Tissue-integrated prostheses osseointegration in clinical dentistry. Chicago: Quintessence Publishing Co.; 1985. pp. 88–98.
- Zarb GA, Albrektsson T. Osseointegration: a requiem for periodontal ligament? Int J Periodontal Restor Dent. 1991; 11:88–91.
- Parithimarkalaignan S, & Padmanabhan, T. V. Osseointegration: An Update. The Journal of the Indian Prosthodontic Society. 2013. 13(1), 2–6. http://doi.org/10.1007/s13191-013-0252-z
- Alghamdi, H. S. Methods to Improve Osseointegration of Dental Implants in Low Quality (Type-IV) Bone: An Overview. Journal of Functional Biomaterials. 2018. 9(1), 7. http://doi.org/10.3390/jfb9010007
- Ajayi, Y. O., Nwachukwu, N., &Akinboboye, B. O. (2017). TREATMENT OUTCOME OF SHORT DENTAL IMPLANTS. Journal of the West African College of Surgeons, 7(4), 52-71.
- Z. Schwartz and B. D. Boyan, “Underlying mechanisms at the bone-biomaterial interface,” Journal of Cellular Biochemistry, 1994. vol. 56, no. 3, pp. 340–347.
- Z. Schwartz, K. Kieswetter, D. D. Dean, and B. D. Boyan, “Underlying mechanisms at the bone-surface interface during regeneration,” Journal of Periodontal Research, 1997. vol. 32, no. 1, part 2, pp. 166–171.
- Z. Schwartz, C. H. Lohmann, J. Oefinger, L. F. Bonewald, D. D. Dean, and B. D. Boyan, “Implant surface characteristics modulate differentiation behavior of cells in the osteoblastic lineage,” Advances in Dental Research, 1999. vol. 13.
- D. Buser, T. Nydegger, T. Oxland et al., “Interface shear strength of titanium implants with a sandblasted and acid-etched surface: a biomechanical study in the maxilla of miniature pigs,” Journal of Biomedical Materials Research, 1999. vol. 45, no. 2.
- D. Buser, R. K. Schenk, S. Steinemann, J. P. Fiorellini, C. H. Fox, and H. Stich, “Influence of surface characteristics on bone integration of titanium implants. A histomorphometric study in miniature pigs,” Journal of Biomedical Materials Research, 1991. vol. 25, no. 7.
- Ma T., Ge X., Zhang Y., Lin Y. Effect of Titanium Surface Modifications of Dental Implants on Rapid Osseointegration. In: Sasaki K., Suzuki O., Takahashi N. (eds) Interface Oral Health Science 2016. 2017. Springer, Singapore
- Kasat, V., &Ladda, R. Smoking and dental implants. Journal of International Society of Preventive & Community Dentistry, 2012. 2(2), 38–41. http://doi.org/10.4103/2231-0762.109358
- Gómez-de Diego, R., Mang-de la Rosa, M. del R., Romero-Pérez, M. J., Cutando-Soriano, A., & López-Valverde-Centeno, A. Indications and contraindications of dental implants in medically compromised patients: Update. Medicina Oral, Patología Oral Y Cirugía Bucal, 2014. 19(5), e483–e489. http://doi.org/10.4317/medoral.19565
- Mellado-Valero A, Ferrer-García JC, Herrera-Ballester A, Labaig-Rueda C. Effects of diabetes on the osseointegration of dental implants. Med Oral Patol Oral Cir Bucal 2007;12:E38-http://www.medicinaoral.com/medoralfree01/v12i1/medoralv12i1p38.pdf
- Mishra SK, Chowdhary R. Heat Generated by Dental Implant Drills During Osteotomy—A Review: Heat Generated by Dental Implant Drills. The Journal of the Indian Prosthodontic Society. 2014;14(2):131-143. doi:10.1007/s13191-014-0350-6.
- Reddy N, Varun K. Osseointegration- Key Factors Affecting Its Success-An Overview. IOSR Journal of Dental and Medical Sciences (IOSR-JDMS) e-ISSN: 2279-0853, p-ISSN: 2279-0861.Volume 16, Issue 4 Ver. V. April. 2017, PP 62-68 www.iosrjournals.org